The Food and Drug Administration on Wednesday approved the sale of an antibiotic for the treatment of urinary tract infections in women, giving U.S. health providers a powerful new tool to combat a common infection that is increasingly unresponsive to the existing suite of antimicrobial drugs.
The drug, pivmecillinam, has been used in Europe for more than 40 years, where it is often a first-line therapy for women with uncomplicated U.T.I.’s, meaning the infection is confined to the bladder and has not reached the kidneys. The drug will be marketed in the U.S. as Pivya and will be made available by prescription to women 18 and older.
It is the first time in two decades that the F.D.A. has approved a new antibiotic for U.T.I.s, which annually affect 30 million Americans. U.T.I.s are responsible for the single-greatest use of antibiotics outside a hospital setting.
“Uncomplicated U.T.I.s are a very common condition impacting women and one of the most frequent reasons for antibiotic use,” Dr. Peter Kim, director of the Division of Anti-Infectives at the F.D.A.’s Center for Drug Evaluation and Research, said in a statement. “The F.D.A. is committed to fostering new antibiotic availability when they prove to be safe and effective.”
Utility Therapeutics, the U.S. company that acquired the rights to pivmecillinam, said it would be available in 2025. The company is also seeking F.D.A. approval for an intravenous version of the drug that is used for more serious infections and is usually administered in a hospital setting.
Health practitioners said they were elated to have another tool in their arsenal given the growing challenge of antimicrobial resistance, which makes existing medications less effective as pathogens mutate in ways that allow them to survive a course of antibiotics.
The problem, largely an outgrowth of antibiotic overuse around the world, is associated with five million deaths, according to the World Health Organization.
“This is an exciting new possibility for treatment of lower urinary tract infections,” said Dr. Shruti Gohil, a professor of infectious diseases at the University of California, Irvine School of Medicine, and an author of a recent study in JAMA that focused on ways to reduce antibiotic overuse in hospitals. “But I would also say that it is going to be important that we use the drug responsibly in this country so that we don’t breed resistance against it.”
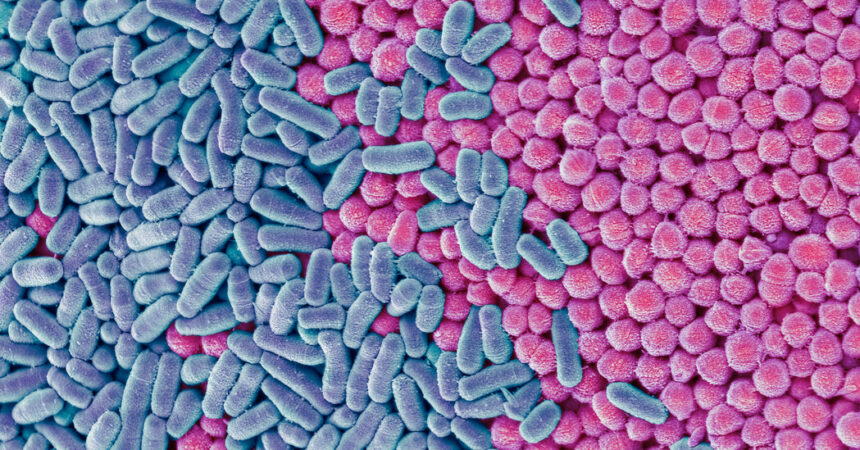
Most U.T.I.s occur when bacteria like E. coli travel from the rectum, genital area or vagina into the urethra and enter the bladder. As they multiply, the pathogens can cause abdominal cramping, burning and bloody urination.
More than half of all women in the United States will acquire a U.T.I. in their lifetime, compared with 14 percent of men. That is in large part because of the differing architecture of the urinary tract in the sexes: Women have shorter urethras than men, which makes it easier for bacteria to reach the urinary tract.
The majority of U.T.I.s are now resistant to one or more antibiotics; ampicillin, once a common treatment, has been largely abandoned. Infections that travel to the kidneys or that enter the bloodstream are more difficult to treat and more dangerous.
People with weakened immune systems or chronic medical conditions are usually the most vulnerable to drug-resistant infections. But U.T.I.s have a dubious distinction: They are the single biggest risk to healthy people from drug-resistant germs.
In the four decades since it was first approved for use in Europe, Pivmecillinam has been prescribed more than 30 million times, mostly in Nordic countries, with few reported complications.
The F.D.A. said that nausea and diarrhea were the most common side effects in the clinical trials that paved the way for pivmecillinam’s approval in the United States.
Tom Hadley, the president and chief operating officer of Utility Therapeutics, said his company moved to acquire the U.S. rights to pivmecillinam after Congress, in 2012, granted an additional five years of exclusivity to manufacturers of new antimicrobial drugs.
Henry Skinner, the chief executive at the AMR Action Fund, a venture capital fund that invested in Utility Therapeutics’ bid to bring pivmecillinam to the U.S., said he was gratified by the F.D.A.’s approval but said the long-term prognosis for new antimicrobial drugs remained grim. The $1 billion fund, financed by the pharmaceutical industry, invests in biotech start-ups working on promising antimicrobials.
Most of the nation’s biggest drug makers, unable to turn a profit on antibiotics, have long since abandoned the field, he said, and the dearth of investment has prompted an exodus of talented researchers.
A federal initiative that would create a subscription-based model for antibiotic development has been languishing in Congress. The $6 billion measure, the Pasteur Act, would provide pharmaceutical companies an upfront payment in exchange for unlimited access to a drug once it is approved by the F.D.A.
Mr. Skinner said he was haunted by one recent estimate suggesting that drug-resistant infections could claim 10 million lives by 2050.
“There are definitely bright spots,” he said. “But more people are dying today than ought to be because we are moving backward, and not delivering the physicians, drugs and diagnostics needed to address the crisis of antimicrobial resistance.”