An independent advisory panel of the Food and Drug Administration rejected the use of MDMA-assisted therapy for post-traumatic stress disorder on Tuesday, highlighting the unparalleled regulatory challenges of a novel therapy using the drug commonly known as Ecstasy.
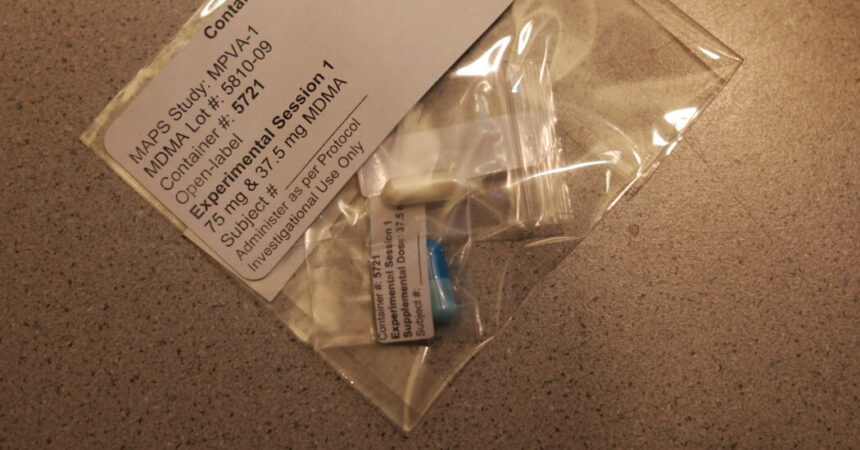
Before the vote, members of the panel raised concerns about the designs of the two studies submitted by the drug’s sponsor, Lykos Therapeutics. Many questions focused on the fact that study participants were by and large able to correctly guess whether they had been given MDMA, also known by the names of Ecstasy or molly.
The panel voted 9-2 on whether the MDMA-assisted therapy was effective, and voted 10-1 on whether the proposed treatment’s benefits outweighed its risks.
Other panelists expressed concerns over the drug’s potential cardiovascular effects, and possible bias among the therapists and facilitators who guided the sessions and may have positively influenced patient outcomes. A case of misconduct involving a patient and therapist in the study also weighed on some panelists’ minds.
Many of the committee members said they were especially worried about the failure of Lykos to collect detailed data from participants on the potential for abuse of a drug that generates feelings of bliss and well-being.
“I absolutely agree that we need new and better treatments for PTSD,” said Paul Holtzheimer, deputy director for research at the National Center for PTSD, a panelist who voted no on the question of whether the benefits of MDMA-therapy outweighed the risks.
“However, I also note that premature introduction of a treatment can actually stifle development, stifle implementation and lead to premature adoption of treatments that are either not completely known to be safe, not fully effective or not being used at their optimal efficacy,” he added.
While the vote is not binding on the F.D.A., the agency often follows the recommendations of its advisory panels. A final decision by the agency is expected in mid-August.
MDMA, or methylenedioxymethamphetamine, also sometimes referred to as midomafetamine is a synthetic psychoactive drug that fosters self-awareness, feelings of empathy and social connectedness.
The illegal drug is listed as a Schedule I substance, defined as having no accepted medical use and a high potential for abuse. Should it win F.D.A. approval, federal health authorities and Justice Department officials would have to follow certain steps to downgrade the drug’s listing, much like the process now underway with cannabis.
The D.E.A. might also set production quotas for the drug ingredients, as it does with stimulant medications used to treat ADHD.
With the panel’s focus on such topics as “euphoria,” “suicidal ideation” and “expectation bias,” the daylong session on Tuesday demonstrated the nuances and complexities facing regulators as they grapple with the terra incognita of a therapy that only recently entered mainstream psychiatry after the nation’s decades-long war on drugs.
An added wrinkle: the F.D.A. is a regulator of medications. It does not regulate psychotherapy and has not evaluated drugs whose efficacy is tied to talk therapy.
If approved, MDMA-assisted therapy would be the first new treatment for PTSD in nearly 25 years. The condition, which affects some 13 million Americans, has been implicated in the outsized suicide rates among military veterans, whose suffering has galvanized lawmakers from both parties and prompted a sea change in public attitudes about therapies reliant on psychedelic compounds.
According to the studies submitted by Lykos, patients who received MDMA plus psychotherapy reported significant improvements in their mental health. The most recent drug trial found that more than 86 percent of those who took MDMA achieved a measurable reduction in severity of their PTSD symptoms.
About 71 percent of participants improved enough that they no longer met the criteria for a diagnosis. Of those who took the placebo, 69 percent improved and nearly 48 percent no longer qualified for a PTSD diagnosis, according to the submitted data.
The questions, concerns and evident skepticism voiced by the 10-member panel echoed those raised by agency staff members, who last week issued a briefing document aimed at helping the panel evaluate the efficacy and potential adverse health effects of MDMA therapy.
In her opening remarks, Dr. Tiffany Farchione, director of the F.D.A.’s division of psychiatry, noted the regulatory challenges posed by MDMA, saying “we’ve been learning as we go along.” But in her testimony and in staff documents, she and other agency officials repeatedly noted that the overall study results were significant and lasting.
“Although the application presents a number of complex review issues, it does include two positive studies in which participants in the midomafetamine arm experienced statistically significant and clinically meaningful improvement in their PTSD symptoms,” she said. “And that improvement appears to be durable for at least several months after the end of the acute treatment period.”
Much of the criticism about Lykos’s study designs focused on so-called functional unblinding, a problem that affects many studies involving psychoactive compounds. Although the roughly 400 patients who took part in the studies were not told whether they had received MDMA or a placebo, to reduce the odds of bias in the results, the vast majority were acutely aware of any altered state of mind, leading them to correctly guess which study arm they were enrolled in.
The F.D.A., which worked with Lykos to design the trials, has acknowledged shortcomings in the study designs and recently issued new guidance to address the issues facing psychedelic researchers.
A number of other critical voices emerged in recent months. They include the Institute for Clinical and Economic Review, a nonprofit that examines the costs and effectiveness of medications, which issued a report calling the effects of the treatment “inconclusive” and questioning Lykos’s study results.
Other organizations, like the American Psychiatric Association, have not opposed approval outright, but have called on the F.D.A. to mitigate any potential negative consequences by crafting rigorous regulations, strict prescribing and dispensing controls, and close monitoring of patients.
The F.D.A. staff analysis recommended that approval should be contingent on restricted health care settings, monitoring of patients and diligent reporting of adverse events.
Just before they voted on Tuesday, the advisory panel heard from more than 30 speakers who offered starkly divergent views on the application.
Several critics focused on Rick Doblin, a veteran psychedelics advocate who in 1986 founded the Multidisciplinary Association for Psychedelic Studies, the nonprofit organization that filed the original application for MDMA-assisted therapy with the F.DA. The organization later created a for-profit entity that earlier this year became Lykos.
Brian Pace, a lecturer at Ohio State University, described the company applying for approval as a “therapy cult” and criticized Mr. Doblin’s public comments highlighting his zeal for psychedelics, including a belief that legalizing and regulating them would bring about world peace.
But the majority of those who spoke in favor of the application offered deeply personal accounts of how MDMA-therapy had largely quieted the symptoms of their PTSD.
Among them was Cristina Pearse, who said she suffered from PTSD after being sexually assaulted when she was 9. Over the years, she said she had been prescribed a litany of psychiatric medications and at one point she attempted suicide.
MDMA therapy, she said, changed her life. “What used to feel like a tsunami of overwhelming panic was now merely a puddle at my feet,” said Ms. Pearse, who started an organization that helps women recovering from trauma.
She ended her testimony by urging the F.D.A. to approve the application.
“How many more people need to die before we approve an effective therapy?” she asked. “As you weigh the risk, please keep in mind that this therapy can save many lives. I lost most of my life to this disease. I’m grateful to reclaim it now. But I wish this was an approved medication decades ago.”